A Mathematical Model Suggests COVID-19 Is Far From Controlled in Venezuela
Although the number of COVID-19 cases hasn’t collapsed Venezuela's health system yet, there's reason to believe that the worst is about to come


Photo: Sofía Jaimes Barreto
On May 8th, the National Academy of Physics, Mathematics and Natural Sciences published an 18-page document with their take on the COVID-19 pandemic in Venezuela. This is the first publicly-disclosed mathematical model to estimate the magnitude of the epidemic in the country as well as its possible evolution in the upcoming months.
Numbers from the United Nations Office for the Coordination of Humanitarian Affairs (OCHA) indicate that at the time the report was written (late April), the Venezuelan government had performed only 5,969 PCR tests, about 1.7% of over 300,000 tests it claimed to have carried out. The number represents 21 tests per 100,000 people, nine times less than Ecuador, one of the most badly-hit countries in the region. With so few PCR tests and, as we argued a couple of weeks ago, it isn’t surprising that Venezuela reports a low number of official cases.
The disease is underdiagnosed. But to what extent?
To answer that question, the authors of the report used a mathematical model developed earlier this year by the London School of Hygiene and Tropical Medicine, one of the leading public health institutions in the world.
The model uses the date of the first confirmed death and the approximate Case Fatality Rate (CFR) of the disease to estimate the number of probable cases at that point in time. Although the math behind the analysis might look complex, the idea is simple: If you know the proportion of people who die of the disease, you can estimate the number of people who were sick when the first fatalities were reported. This approximation shows that when a death is confirmed in a location, there are already many more cases.
This makes sense if you consider the overall mortality rate of COVID-19 is quite low—only 2% of the total number of cases will end up dying.
In an optimistic scenario where the disease’s R0 is 1.2 (a number close to one, which means the disease spreads slowly), and it has a large CFR (which means that deaths represent a larger proportion of all cases), the model suggests that by March 30th, we should have had about 289 cases rather than the 135 officially reported then. If we assume less ideal scenarios (a high R0 and low CFR), the estimation goes all the way up to 800 cases.
The disease is underdiagnosed. But to what extent?
The real number was probably somewhere in between, and it indicates that at least until early April, the epidemic, although underdiagnosed, was not particularly massive. This still seems to be the case, as can be inferred by the simple fact that Venezuelan hospitals have not collapsed… yet.
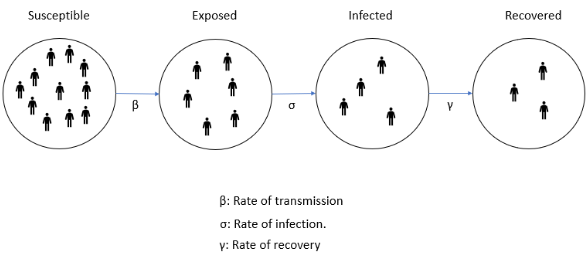
Now, with further epidemiological characteristics of the disease you can make an educated guess of the total infected people you’ll have at any point of time. This is done using a SEIR model, which divides the total population in four compartments (Susceptible, Exposed, Infected and Recovered) and estimates the size of each group at any point in time, based on the rate at which people from one group move to another. Again, the math is tricky, but the basic idea is simple.
For any given day, you’ll have a pool of susceptibles. A proportion of this group, defined by the virus transmission rate, will become exposed. A proportion of this second group, defined by the rate of infection, will become infected. Finally, every day, a proportion of these infected, defined by the rate of recovery, will recover.
All these variables will define the evolution of the R0, which will in turn determine the pace at which cases increase or decrease. This new number, Re (as R0 is known when it changes over time), will vary as the epidemic evolves. If Re is >1, the cases will increase; if it’s <1, cases will decline.
From this point on, the number of infected will grow based on the value of the rates previously described. While the rate of infection is somewhat constant, depending on the biological characteristics of the virus, the other two can change quicker. The rate of recovery can increase by reducing the period an individual is infectious with a specific treatment, like promising drugs, such as remdesivir.
The rate of transmission, which defines the number of people exposed, will depend on the interventions in place at a particular moment. Social distancing and quarantine are effective in reducing it, but once they are lifted or people ignore them, it can rebound. And so will Re.
This behavior, characteristic of low-income countries, is particularly true in Venezuela, where the vast majority of the population can’t sustain long quarantines
With the proper data, SEIR models can “predict” the number of patients that will exist at a particular moment. But these predictions are based on several assumptions, which are not necessarily true.
In the model run by the Academy, authors assumed the initial number of cases was low. Venezuela has been under a relative “quarantine” from the rest of the world for a couple years now, when most airlines stopped flying to the country. Restrictions on the few commercial flights still landing were also announced early by chavismo.
The transmission rate of the model also starts low, as quarantine measures dictated by the government were initially followed by the majority. But it progressively grows, as people are forced to get back to work to survive. This behavior, characteristic of low-income countries, is particularly true in Venezuela, where the vast majority of the population can’t sustain long quarantines, especially when the epidemic appears to be controlled, both by its slow onset, and considerable underdiagnosis.
In a few words, when people stop taking the disease seriously enough.
Based on this assumption, the Academy of Sciences reaches a daunting conclusion: In the best case scenario, where the Re increases slowly and discretely, Venezuela would reach a peak of 1,000 new cases per day by early September. In the worst case (a substantial increase in Re), the peak comes in July and reaches 4,000 new cases per day, comparable to the current situation in the United Kingdom or Spain.
There’s no need to highlight how complicated this scenario would be to handle for a health system with less than 200 ventilators. Nonetheless, we can’t forget models are just that, an imperfect approximation to reality. To build them, we must assume a lot of things that might be different in reality.
We don’t know, for instance, how quickly Re would increase in Venezuela. Even if quarantine measures are lifted (or ignored), the disease seems to be spreading particularly slowly in the country. The recent fuel crisis, as well as the long-standing economic collapse of the country have already limited the level of social interaction considerably, and might be partially responsible for this situation. In any case, accurately predicting the peak of transmission, or the future behaviour of a disease is extremely difficult, particularly during the initial, non-exponential period, where Venezuela seems to be standing right now.
Even in the worst case scenario, given Venezuelan demographics, the death toll might not be as high as in some developed countries, where elderly folks are a big proportion of the total population and a higher number of infected will end up requiring hospitalization or ventilation. Brazil and Ecuador, however, are cautionary tales of the effect the virus can have in “young countries,” even with fairly functional health systems.
Beyond that, the Academy’s model confirms several suspicions: First, COVID-19 is certainly underdiagnosed in Venezuela (authorities could be missing between 63% to 95% of all cases), as a consequence of the low PCR testing capacity. Second, the country is still in the initial stages of the epidemic and the low progression we have experienced so far doesn’t mean it will be spared from the worst in the future.
Assuming COVID-19 has been controlled in Venezuela (as Maduro repeats) is a mistake, and so is the idea that the disease is a hoax engineered by the regime to furtherly control the population. There is no doubt Maduro is exploiting the situation, but COVID-19 is a real danger and social distancing measures have to be maintained. The limited impact the disease has had so far seems more a fortuitous accident than the result of the Venezuelan government’s actions. No steps have been taken to prevent the damage the disease could have in the coming months. A mitigation plan to help the population endure the quarantine hasn’t been created, diagnostic capacity hasn’t been increased, not even water or electricity are guaranteed in most hospitals outside Caracas, not to mention the lack of isolation wards or ventilators.
More importantly, Maduro has refused to provide any guarantee of a peaceful solution to the ongoing political crisis, limiting the country’s response capabilities and access to foreign aid. It’s imperative to address these issues and prepare the country for a peak of cases we will likely see soon, otherwise the quarantine is just postponing the inevitable, while destroying what was left of Venezuelan economy.
Caracas Chronicles is 100% reader-supported.
We’ve been able to hang on for 22 years in one of the craziest media landscapes in the world. We’ve seen different media outlets in Venezuela (and abroad) closing shop, something we’re looking to avoid at all costs. Your collaboration goes a long way in helping us weather the storm.
Donate