Venezuela Threatens Latin America’s Efforts for Eliminating Malaria
The World Health Organization report shows that more than half of malaria cases in the Americas are being recorded in our country, amid the gold rush and the humanitarian emergency


Photo: Pan American Health Organization
The 2020 World Malaria Report was released by the World Health Organization (WHO) last week, and it summarizes epidemiological data, collected from all around the world throughout 2019, describing the current state of the disease globally, listing the most important milestones reached in the last two decades.
This report is particularly important for Venezuelan researchers: because of a lack of regular epidemiological reports in the country, it represents a rare opportunity to glimpse into official malaria figures.
Venezuelan authorities reported to WHO that 462,338 cases of malaria originated in the country last year, a number slightly larger than the one reported in 2018 (453,041). The number of reported deaths has decreased from 333, when it peaked in 2017, to 126 in 2019.
However, these figures must be interpreted carefully, as not all malaria cases are reported by the government, not necessarily because Venezuelan authorities hide cases (which wouldn’t be too surprising), but because not all malaria cases are detected by epidemiological surveillance networks.
To address this, WHO calculates its own estimations, adjusting the number of reported cases by national authorities, for completeness of reporting, the likelihood of having a detectable number of parasites in a blood sample, and the proportion of sick people who don’t seek medical attention. Accounting for these factors, WHO estimates that the true number of malaria cases in Venezuela last year was somewhere between 415,000 and 538,000, with a point estimate of 467,421, which represents 53% of the regional total.
Compared to 2000, when cases were estimated to be around 35,550, this represents an increase of 1,213% in cases and 1,020% increase in population-adjusted incidence.
The Venezuelan reality contrasts progress made elsewhere. Although 229 million cases of malaria and 409,000 deaths were reported around the world during 2019, the numbers reflect the overwhelming global progress made in the last two decades.
In 2000, before game-changing interventions such as insecticide-treated bednets (ITNs) and artemisinin-based treatments, there were 238 million reported malaria cases and 736,000 deaths, even though the global population at risk was considerably smaller than today.
The creation of new funding schemes and an unprecedented political will, particularly in African countries (where 94% of all malaria cases still occur) have been key to secure this success. Although global progress has somewhat stalled, a similarly positive picture can be seen in many other regions. Malaria incidence rates (calculated per 1,000 people at risk) in Southeast Asia reduced by 78%, compared to 2000, 50% in the Eastern Mediterranean (which also includes parts of Africa), 60% in the Pacific, and 53% in the Americas.
But the situation in the latter requires a more in-depth look. Despite being an important public health problem, malaria cases in the Americas represent only 0.38% of the global disease burden and are strongly focalized around the Amazon basin. Yet, the region as a whole is far from reaching its malaria elimination goals. The incidence in the Americas has declined from 1.5 million in 2000 to 0.9 million in 2019, but this trend has reversed in the last five years, undoubtedly, due to cases increasing in Venezuela.
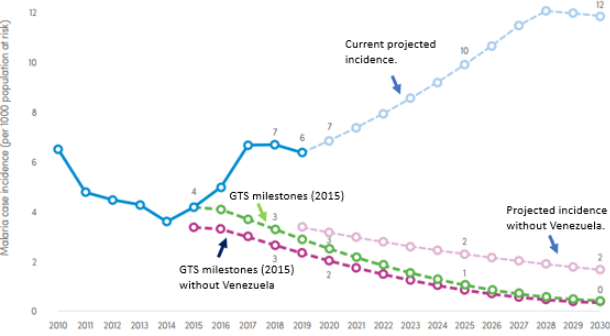
Current and projected progress in malaria control in the WHO region of the Americas.
Photo: WHO’s World Malaria Report.
The figure above is particularly telling, as it shows that if it were not because of Venezuela, the Americas would only be 15% off the regional incidence target set by WHO’s Global Technical Strategy (GTS) for malaria for the 2016-2030 period, rather than the current 45%.
A similar situation occurs with malaria mortality. Although the Americas’ mortality rate is low compared to other regions (0.4 deaths per 100,000 people at risk), WHO estimates that at least 400 people died of malaria in Venezuela during 2019. This might look like a somewhat negligible number compared to the global total of 400,000; but it represents 73% of all estimated deaths in the region, and a mortality rate of 2.82 deaths per 100,000 people at risk, seven times higher than the regional rate.
The main reason for this situation is underinvestment and negligence. Venezuela is second only to French Guiana, in the list of countries or territories in the region that invested the least in malaria control. While places like Suriname invested $12 per person at risk, Venezuela invested a couple of cents. Similarly, the Venezuelan government has made no efforts to limit illegal mining in Bolívar, a key driver in the resurgence of the disease in many other states; or to guarantee regular access to antimalarial treatment to particularly vulnerable groups, such as southern indigenous tribes.
Not all is terrible though. The scale of certain interventions increased. Distribution of ITNs for instance, went from 5,000 in 2017, to 256,311 in 2019, and the number of rapid diagnostic tests, from 48,000 in 2018 to 250,000 a year later.
These measures have been almost entirely implemented and funded by international agencies like the Pan American Health Organization (PAHO), or NGOs such as Médecins sans Frontières (MSF), the Rotary Club, and the International Committee of the Red Cross (ICRC), who moved forward to occupy the vacuum left by the Venezuelan State. These interventions remain restricted to high-transmission pockets in mining areas of Bolívar, and to a lesser extent, Amazonas, and don’t substitute a well-structured and functioning malaria national control program. Nonetheless, they’ve certainly had an impact, and will likely translate into a reduction in the number of cases reported in 2020.
Also, while disruptions in health coverage caused by the COVID-19 pandemic threaten to severely undermine recent progress on malaria control in many lower-middle-income countries (LMIC), their effect in Venezuela is harder to foresee.
Malaria remains a heavily focalized problem in the country, with most cases originating from mining activity in Bolívar. Reduced access to healthcare services could definitely lead to more malaria deaths this year, particularly in remote areas where indigenous groups might be disproportionately affected. However, mobility restrictions caused by quarantine measures (and widespread shortages of fuel) have almost certainly reduced the number of people traveling to high-transmission areas, and therefore, the transmission of disease.
As most of the resources of the already overstretched Venezuelan medical system are channeled into management of COVID-19, the number of cases of malaria diagnosed, and therefore reported by authorities to the WHO, will probably reduce this year as well, as in fact, many Venezuelan malariologists already anticipate.
Clearly, neither the brave effort of NGOs nor an ongoing pandemic, can solve the malaria problem in Venezuela. Experience from other countries (and from Venezuela itself) shows that extensive funding, and particularly political will and commitment are indispensable, and will be fundamental for the malaria tide in Venezuela to turn. Without this, limited interventions are welcome and needed, but are unlikely to achieve any sustainable success.
Caracas Chronicles is 100% reader-supported.
We’ve been able to hang on for 22 years in one of the craziest media landscapes in the world. We’ve seen different media outlets in Venezuela (and abroad) closing shop, something we’re looking to avoid at all costs. Your collaboration goes a long way in helping us weather the storm.
Donate




